In creating the immune system map, scientists from the Wellcome Sanger Institute and ETH Zürich show how immune cells across the body link up and communicate.
This research, published on 3 August 2022 in Nature, includes the discovery of many previously unknown interactions that together shed light on the organisation of the body’s immune defences. This offers answers to longstanding questions about current immunotherapies that are already used to treat patients. In the future, this public and detailed immune system map could also be vital in identifying new therapies.
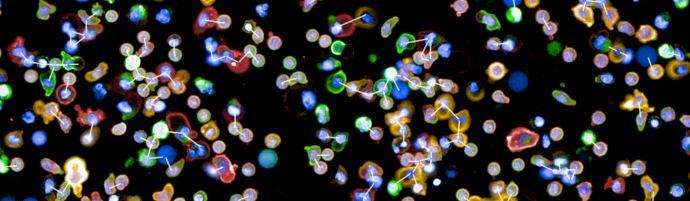
The immune system is made up of specialised cells, some of which individually travel through the body to scan for signs of injury or disease. Once these cells detect a threat, they need to communicate the message to other cells in order to mount an effective immune response. One way this cell-to-cell signalling is done is through proteins on the surfaces of cells that bind on to matching ‘receptor’ proteins on the surfaces of other cells. Previously, scientists and clinicians only had an incomplete map of these receptor connections between all of the different types of immune cells in the body.
An in-depth understanding of the interactions between immune cells, and how this communication fits into the human body as a whole, is vital if we are to develop treatments that enhance the immune system in order to fight disease, known as immunotherapies.
Immunotherapies have already demonstrated great potential in treating disease, most notably with certain cancers. However, these only work well in certain groups of patients and for particular conditions. Knowing the map of immune receptor connections could help explain why immunotherapies sometimes only work in a subset of patients, and offer new targets for designing future immunotherapies that may work for patients who currently do not benefit from these cutting-edge treatments.
It is also necessary to understand the cell-to-cell signals happening in the immune system if we hope to prevent and treat autoimmune diseases, which are caused when the body mistakes internal signals and attacks itself.
This new publication, from the Wellcome Sanger Institute and ETH Zürich, details how researchers isolated and investigated a near-complete set of the surface proteins that physically link immune cells together. They then used a large amount of computational and mathematical analysis to create a map showing the cell types, messengers, and relative speed of each conversation taking place between immune cells.
Creating this detailed map of the immune system has required years of technological advances to tackle a problem of this scale. Each immune cell may have hundreds of distinct surface proteins and receptors on it, and the interactions involving these proteins are often so transient that specialised methods had to be invented to make assembling an accurate map possible.
With this map, it is possible to see the impact of different diseases on the immune system as a whole, and investigate new therapies that bind to different proteins on the immune cell surface. Cell surface proteins serve as the basis for new medicines more often than any other protein type, due to their accessibility to drugs and powerful influence on the signals a cell receives.
Jarrod Shilts, first author from the Wellcome Sanger Institute, said: “Meticulously isolating and analysing every immune cell and their interactions with others has given us the first map of the conversations between all of the immune cells in the human body. This is a huge step in understanding the inner workings of the immune system and will hopefully be utilised by researchers all around the world to help develop new therapies that work with the body’s defence mechanisms.”
Professor Berend Snijder, an author from the Institute of Molecular Systems Biology at ETH Zürich, said: “This research has produced an incredible new tool that can be used to help highlight which proteins and pathways would be beneficial to target in drug development. It can also give insight into whether a drug will have impact on other pathways, which can cause side effects. All of this information may help in the development of new therapies and could give crucial supporting evidence to help ensure that the most effective treatments are put into clinical trials.”
Professor Gavin Wright, senior author previously based at the Wellcome Sanger Institute and now at the University of York, said: “Immunotherapies work with the body’s immune system to combat diseases such as cancer and autoimmunity. They can be incredibly effective in certain groups of people, but not all, leaving some people without treatment. Our research, a culmination of over two decades of work, could hold the key to understanding why these treatments are more effective in some groups, and how they could be adapted to ensure that as many people as possible can benefit from them.”
Image: courtesy of Wellcome Sanger Institute