Researchers from the Wellcome Sanger Institute, the Olivia Newton-John Cancer Research Institute in Australia, and collaborators, have identified specific strains of bacteria that are linked with a positive response to combination immunotherapy in the largest study of its kind.
The study, published today (1 March) in Nature Medicine, details a signature collection of microorganisms in an individual’s gut bacteria that may help identify those who would benefit from combination immunotherapy and help explain why the efficacy of this treatment is otherwise hard to predict.
In the future, understanding more about these bacteria strains can help drive the development of next-generation probiotics, known as ‘live biotherapeutic products’, that focus on modulating the microbiome to support combination immunotherapy from the inside.
Immunotherapy is a type of treatment that harnesses the body’s immune system to target the cancer. While it can be very effective, it only works in a proportion of recipients across a wide range of cancers. As with all cancer treatments, immunotherapy can have multiple side effects. Therefore, being able to predict who is most likely to respond to treatment helps ensure that patients do not endure these unnecessary side effects for no medical benefits.
This study used samples collected in a large, multi-centre Australian clinical trial where combination immunotherapy was effective in 25 per cent of people with a broad range of advanced rare cancers, including rare gynaecological cancers, neuro-endocrine neoplasms, and upper gastrointestinal and biliary cancers.
The clinical trial focused on a type of combination immunotherapy known as immune checkpoint inhibitors. These anti-cancer agents block the body’s immune checkpoint proteins, allowing the immune cells to destroy cancer cells. In this case, the immunotherapy blocked the PD-1 and CTLA-4 checkpoints.
Researchers used stool samples from clinical trial patients and performed deep shotgun metagenomic sequencing1 to map all the organisms within the participants’ microbiomes, down to the strain-level.
They discovered multiple strains of bacteria in those who responded well to treatment, many of which had not been cultivated before. This allowed them to identify a microbiome signature that was found in patients who responded well to treatment.
In addition to this, the team used this signature to train a machine learning model that could predict who would benefit from combination immunotherapy.
They conducted a meta-analysis of previous studies and found that their signature can be applied to different cancers, such as melanoma, and across countries, to predict individuals whose cancer will likely respond to combination immunotherapy.
However, when applied to patients who received just one of the immunotherapy drugs, targeting the immune checkpoint receptor PD-1 only, the machine-learning model could not identify those who would respond to treatment.
This suggests that the relationship between gut microbiota and treatment response is specific for particular therapeutic combinations. The researchers therefore suggest that future development of diagnostics tests or therapeutics that rely on the gut microbiome should be tailored to the immunotherapy regimen, regardless of cancer type.
This step towards personalised medicine may help extend cancer treatments to more people and can match individuals to therapies that would benefit them the most.
Dr Ashray Gunjur, first author from the Wellcome Sanger Institute and the Olivia Newton-John Cancer Research Institute, Australia, said: “Our study shows that understanding the microbiome at strain-level, not just species-level, can open up a new level of personalised medicine. Having that extra resolution is crucial if we are to understand what is happening in the human body and the interplay between cancer treatment and the microbiome. Being able to test the specific mechanisms of this relationship between specific strains and response is the next horizon in this research, and one that could benefit human health in a multitude of ways.”
Dr David Adams, co-senior author from the Wellcome Sanger Institute, said: “Rare cancers can be hard to study and treat and while immunotherapy treatment can be incredibly effective in some of these cases, it can also be unpredictable. Our research shows that the microbiome impacts how well someone responds to combination immunotherapy, but that monotherapy gives a different result. This suggests that the microbiome should be taken into account when developing therapeutics going forward. In addition to this, there is a possibility of developing live biotherapeutic products that could provide the bacteria shown to support immunotherapy, helping the microbiome work with the patient to give them the best odds of response possible.”
Dr Trevor Lawley, co-senior author from the Wellcome Sanger Institute, said: “Our microbiomes vary from person to person, all of us containing a different ecosystem of bacteria and other organisms that shape our responses to the world around us. Our research highlights how an individual’s microbiome can predict how they will respond to cancer treatment, which can have a direct clinical impact by identifying those that would benefit the most, and aid in the design of future clinical trials.”
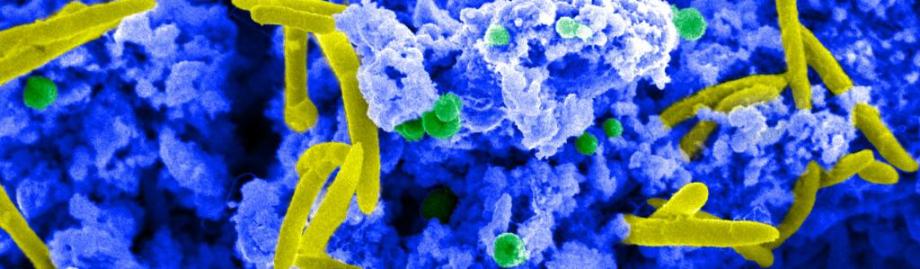
Image: Courtesy of Dave Goulding, Wellcome Sanger Institute