Researchers from the Wellcome Sanger Institute and their collaborators at Ghent University, Belgium, the National Institutes of Health’s National Institute of Allergy and Infectious Diseases and others, uncovered key differences in the development of immune cells. This understanding could help scientists engineer immune cells outside the body to fight cancer, counter age-related immune decline, or prevent transplant rejection risks.
The study, published today (20 November) in Nature, is part of the international Human Cell Atlas (HCA) initiative to map every cell type in the human body1. Insights gained from studying how thymus samples change before and after birth could help future researchers generate an artificial thymus, the first step in being able to engineer therapeutic immune cells for older adults or people with compromised immune systems.
This paper is one of a collection of more than 40 HCA publications in Nature Portfolio journals that represent a milestone leap in our understanding of the human body.
The immune system protects the body from infections and cancer with the help of a diverse array of T cells, a type of white blood cell. T cells must first be trained to recognise threats without attacking the body’s own healthy cells. The thymus, a small organ behind the breastbone, is where this crucial T cell training occurs.
When the thymus malfunctions, it can result in weakened immunity or autoimmune diseases, where the body mistakenly attacks itself, leading to conditions such as type 1 diabetes or rheumatoid arthritis.
Despite its importance, little is known about the early development of the thymus, as it uniquely functions primarily during infancy and then gradually degenerates over the lifespan2. Studying its early stages could allow us to understand why immunity wanes with age, leaving older adults vulnerable to infection and less responsive to vaccines3.
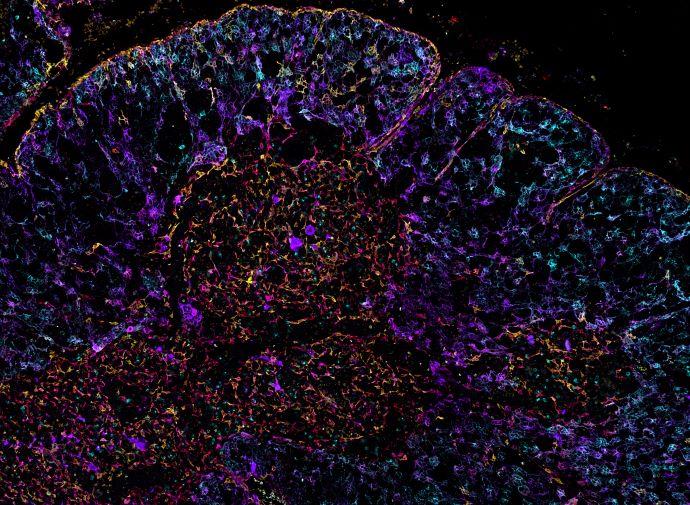
In this new study, researchers from the Wellcome Sanger Institute and their collaborators tracked thymus and T cell development in samples ranging from eleven weeks post-conception to three years old4 using single cell sequencing and advanced spatial mapping techniques.
They discovered that the organ’s basic structure and function is established as early as twelve weeks post-conception, suggesting that early pregnancy factors may have a more profound impact on lifelong immune function than previously recognised.
The team uncovered key differences in the development of various T cells types5 — some that help orchestrate immune responses by directing other immune cells and others that directly attack infected or cancerous cells. This understanding could inform new T cell engineering therapies that selectively boost immunity for cancer treatments or suppress it for autoimmune conditions and transplants.
The researchers also discovered locations of progenitor cells that give rise to important supporting cells in the thymus which also mimic the body’s own environment so that T cells would not react to self. This could help researchers in the future to create an artificial thymus for regenerative immune therapies for older adults or people with compromised immune systems.
A key achievement of the study was the creation of a standardised high resolution spatial mapping method called OrganAxis to compare the composition and structural organisation of thymus samples across various stages of development at a much higher resolution than ever before. This approach could be applied to other organs that change significantly over time or vary widely across individuals, such as the liver or kidneys.
Dr Nadav Yayon, co-first author of the study formerly at the Wellcome Sanger Institute and EMBL-EBI, and now based at the Cambridge Stem Cell Institute, University of Cambridge, said: “The thymus is uniquely crucial in setting up lifelong immunity, but until now, comparing its different developmental stages was almost impossible, as they appeared like completely different organs. OrganAxis lets us integrate different spatial datasets to uncover hidden properties that go unnoticed when viewed individually. Using key structures as reference points, much like a hiker uses landmarks to navigate, we now see how structures are formed early on, enabling us to track T cell training over time.”
Dr Veronika Kedlian, co-first author of the study formerly at the Wellcome Sanger Institute, and now based at the Cambridge Stem Cell Institute, University of Cambridge, said: “Our atlas of healthy thymus development could lead to new strategies for boosting immunity, particularly in older adults or those with thymus deficiencies. We are already applying this resource to study age-related immune changes and conditions like DiGeorge syndrome, where children are born without a functioning thymus and are highly vulnerable to infections.”
Dr Sarah Teichmann, senior author of the study and co-founder of the Human Cell Atlas, formerly at the Wellcome Sanger Institute, and now based at the Cambridge Stem Cell Institute, University of Cambridge, said: “This thymus map is the first full model of a human organ at single cell resolution and transcriptomic breadth. It represents a crucial piece of the puzzle in our effort to understand human biology cell by cell in the Human Cell Atlas. By understanding how the thymus educates immune cells from their earliest stages, we are opening up insights into immune deficiencies and autoimmune conditions. The map offers an important perspective for developing therapies to strengthen or correct immune responses.”
Image: Human Thymus Rainbow. Andrea Radtke